September 7, 2016
How More Virginia Women Could be Treated for Maternal Depression
More women who suffer from untreated maternal depression could get the help they need if Virginia lawmakers would say yes to expanding Medicaid and accepting the federal funds that would come with it.
Maternal depression hurts women and their children, according to a recent report from the Center for Children and Families at Georgetown University. While effective treatments for depression are available, they remain out of reach for mothers who lack health insurance and those struggling to make ends meet. The Affordable Care Act gave states options to cover more adults by expanding Medicaid, helping more women get the care they need. But, Virginia lawmakers have yet to take action, leaving more than 100,000 women without health care coverage.
Making sure mothers get quality, affordable health care and treatment for maternal depression is necessary for children’s healthy development and future success. Untreated maternal depression is seen as contributing to changes in children’s brain chemistry, learning disabilities, social disorders, and difficulty in dealing with stress. When states expand Medicaid, children have the opportunity to receive care from healthier adults and improve their chances of breaking the cycle of generational poverty.
Depression is treatable. But many mothers go without treatment because they can’t pay for it. Medicaid provides mothers who lack financial resources or employer-provided health insurance with affordable coverage. That means they are more likely to get necessary screenings and treatments for maternal depression. But, in states like Virginia that have not expanded Medicaid, only parents in extreme poverty are eligible for coverage.
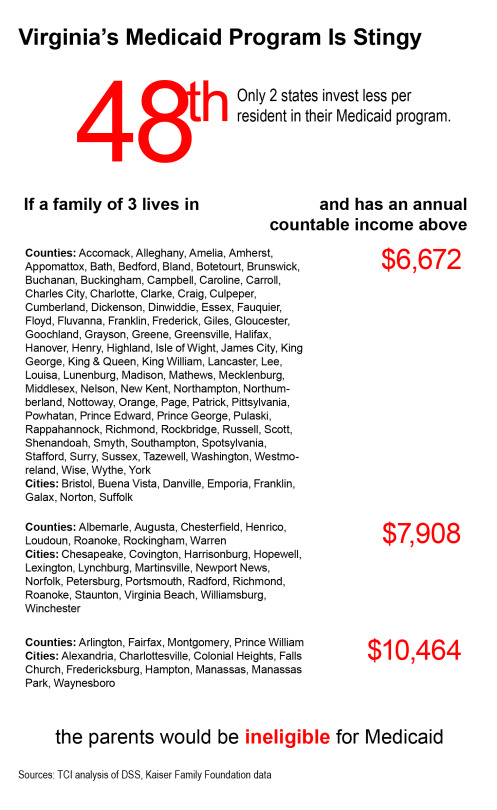
Virginia has one of the stingiest Medicaid programs in the country. Parents in a family of three can’t make more than $10,464, and in some parts of the state it’s even lower. And if they make less than $20,160, they get no help buying insurance on the federal exchange. They’re among the 230,000 Virginians stuck in the state’s coverage gap.
What’s more, Virginia’s patchwork of Medicaid eligibility rules makes maintaining coverage extremely difficult, particularly for pregnant women. In 2015, for example, approximately 53,000 Virginia women had coverage through Medicaid because they were pregnant, according to the most recent data available from the state Medicaid office. But pregnancy-related coverage for women ends 60 days after they give birth. That means these new moms were most likely kicked off Medicaid shortly after they had their babies. However, 60 days often is not enough time to identify and sufficiently treat maternal depression. Closing the coverage gap would mean a mother could have continuous coverage before, during, and after a pregnancy, giving both her and her child the best chance for a healthy future.
Virginia lawmakers have the opportunity to help economically challenged, uninsured moms and their children get the care they need to be healthy and productive. The well-being of all women and children is too important to ignore.
–Kenneth Gilliam, Policy Associate
Category:
Health Care
