August 14, 2024
Virginia’s Medicaid Unwinding Winds Down: A Look at the Numbers and Next Steps to Connect People to Health Coverage
The 59th anniversary of Medicaid’s creation on July 30 was cause to celebrate the program’s immense success, which covers health coverage for millions of adults and children and over 1 in 3 births every year throughout every corner of Virginia. It was also a reminder of the key improvements that advocates have won in recent years to connect more people to coverage and expand access to critical services. We also recognize we are nearing the end of an over-year-long undertaking to redetermine the eligibility of everyone enrolled in Medicaid, which has shifted the health coverage landscape for state agencies, eligibility workers, and — most importantly — Virginia families.
The process to redetermine the eligibility of over 2.1 million people was expected to put a strain on local Department of Social Services (DSS) eligibility workers and state systems with the potential to harm children, Black and Latino individuals particularly. As of August 7, 2024, and as we near the end of this process in Virginia, we know that nearly 238,000 people of color and over 125,000 children ages 18 and under have lost Medicaid coverage. While we don’t know the exact number of children and individuals who remain uninsured due to data limitations, Virginia lawmakers should take action to ensure more accessible pathways to health insurance for those who lost coverage and expand eligibility to coverage for children and families. Additionally, with Virginia’s Department of Medical Assistance Services (DMAS) preparing to shut down its “Eligibility Redetermination Tracker” on August 14, 2024, lawmakers and stakeholders should continue to have access to unwinding data and have a full understanding of the final outcome of the Medicaid unwinding process.
Background of “Medicaid Unwinding”
At the start of the COVID-19 pandemic, the federal government enacted several policies to protect and increase access to comprehensive health coverage. In particular, the 2020 Families First Coronavirus Response Act established a “continuous coverage provision,” which meant that anyone enrolled in health coverage through Medicaid could keep it without needing to undergo an annual review of eligibility. This policy benefited hundreds of thousands of Virginia families by offering ongoing health coverage for people who have been enrolled or newly enrolled in Medicaid coverage since March 2020. However, when the continuous coverage provision expired on April 1, 2023, Virginia, like all other states, began reviewing and redetermining eligibility for all people enrolled in Medicaid. This process has been commonly referred to as “unwinding.”
Total Medicaid Coverage Loss (so far)
Loss of health coverage can considerably impact the health and financial well-being of an individual, child, or family. As of August 7, 2024, out of the over 2 million redeterminations that have occurred, roughly 23% (483,465 people) have been disenrolled from Medicaid coverage with about 72,000 people left to be redetermined. This surpasses 2023 estimates from the Department of Medical Assistance Services (DMAS) before unwinding started, which anticipated anywhere from 14% to 20% of people losing coverage once redeterminations resumed. This also surpassed TCI’s mid-range coverage loss estimates using national projections of 17.4%.
While some have lost coverage because they have requested cancellation (34,163), no longer live in Virginia (30,883), or are deceased (19,602), there is very little available data to suggest that the remaining 398,817 individuals who have lost Medicaid coverage have gained another form of health coverage.
Roughly 76,500 people were determined to be no longer eligible because they no longer met the income or resource eligibility criteria. While this may give some hope that they or someone in their family landed a well-paying job and are now covered by employer-sponsored coverage, the reality is that this is no guarantee of coverage. A combination of part-time jobs, a temporary increase in monthly income through seasonal work, or an employer not offering affordable health coverage could push a family out of Medicaid eligibility and into becoming uninsured.
The state has attempted to connect at least some individuals disenrolled from Medicaid coverage to comprehensive health coverage like that offered on the Affordable Care Act (ACA) marketplace to avoid becoming uninsured. A recent DMAS presentation shared that of those disenrolled from Medicaid coverage, 11,686 individuals were found eligible by the Virginia Insurance Marketplace for a plan, and of those, 8,560 were eligible for a plan and financial assistance. Ultimately, 5,868 individuals who were found eligible chose a plan, and of those, 5,410 individuals chose a plan and financial assistance.
These efforts are promising, but this likely represents only a small portion of those who are disenrolled without having been enrolled in other health coverage. There should be a particular concern for those who lost coverage without fully completing the redetermination process. People who experience this type of closure, also known as “procedural coverage loss,” may still be under the impression they have coverage or could still be eligible for coverage.
Procedural Coverage Loss
A significant and ongoing concern is that people who remain eligible for Medicaid risk losing coverage if they do not respond to requests for information and documents within a given time period. This can happen if families do not receive clear communication about the redetermination process, cannot provide the required documentation needed to complete the review, or cannot easily communicate with local DSS eligibility workers due to strained caseloads or spoken language preference. People who have moved, especially those who have faced several changes in mailing address due to housing instability exacerbated by the pandemic-fueled housing market, and people with limited English proficiency may be at greater risk of being kicked off of coverage for procedural reasons.
According to the DMAS Procedural Closure Dashboard, as of August 7, 2024, 256,560,* cases were terminated and not reinstated within three months due to administrative or procedural reasons such as inability to connect with the enrolled individual, lost mail, barriers to uploading needed documents, and more. Those who had coverage closed due to procedural reasons may still be eligible for Medicaid and may be unaware they have been disenrolled. This leaves a swath of Virginians without insurance and at risk to either forgo or face financial barriers to coverage, treatment, medication, and more. Finding out that your coverage has been terminated at your pediatrician’s office or prescription window and needing to pay out of pocket to receive the care or treatment you need can be devastating and financially out of reach for many.
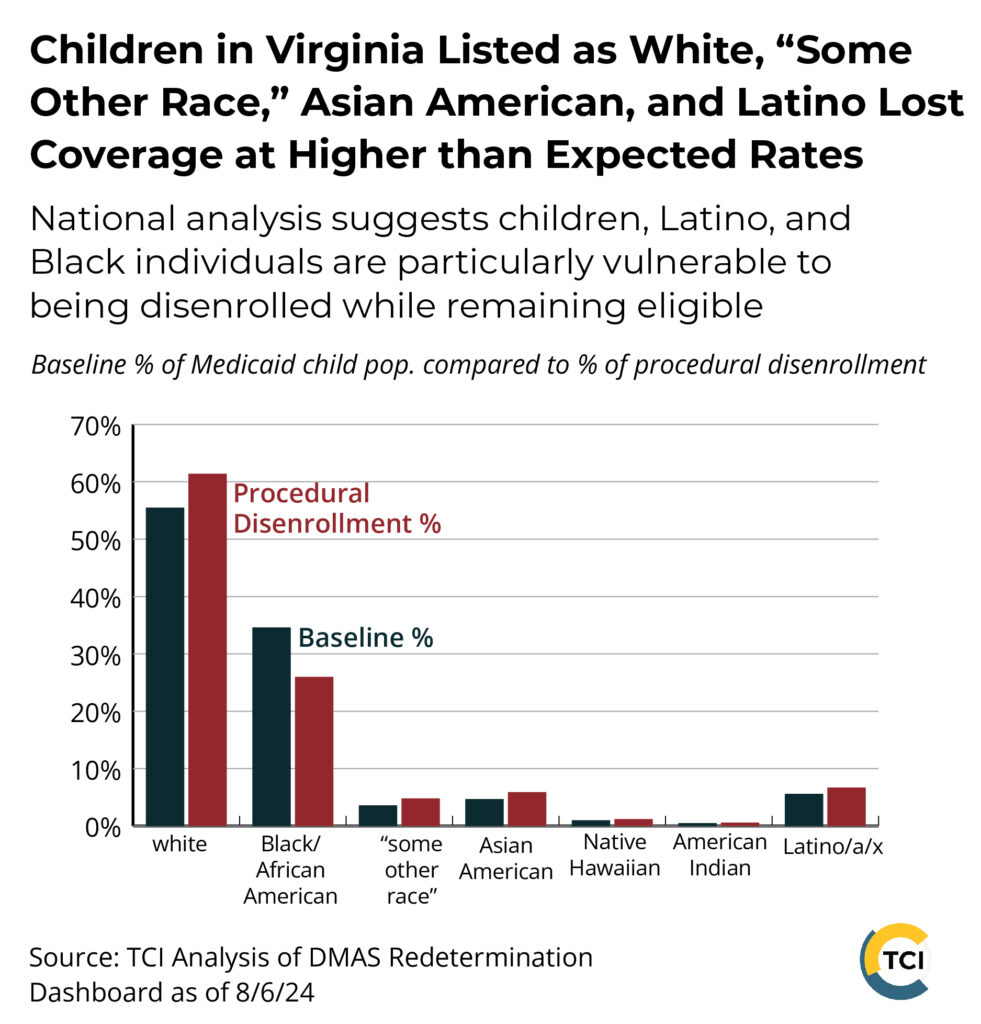
Just over 67,500 cases closed for procedural reasons and not reinstated within three months are those of children ages 18 and under. And nearly 127,000 of the total cases closed for procedural reasons and not reinstated within three months were those of people of color. When comparing procedural disenrollment of children to the baseline population, children listed as white, “some other race,” Asian, and Latino/Hispanic are overrepresented. National analysis suggests children, Latino, and Black individuals are particularly vulnerable to being disenrolled while remaining eligible.
*According to DMAS there may be instances where an individual lost coverage procedurally multiple times. Due to this, we will not be comparing procedural coverage loss numbers to total coverage loss numbers. Of note, the DMAS Closed Members Dashboard currently lists procedural closures at 223,570 cases.
Where We Go From Here
Virginia’s expansion of Medicaid in January 2019 and pandemic-related federal protections drastically increased health coverage options and coverage for Virginia residents. Yet Virginia still ranks only 21st (tied with North Dakota and Illinois) for health coverage rates for people aged 64 and under and 25th (tied with Wisconsin) for children’s (aged 18 and under) health coverage rates.
It may take several months to calculate Medicaid coverage loss and even longer to fully understand the implications for uninsured rates, but the impact and strain on Virginia’s health safety net and the health and well-being of our loved ones and neighbors will be more immediate. While we applaud recent investments in Medicaid eligibility systems and language access to state agencies, Virginia lawmakers should act in the coming legislative session to ensure all income-eligible children have access to affordable health coverage regardless of their immigration status and continue funding targeted outreach and engagement efforts. Otherwise, coverage loss due to Medicaid unwinding could put Virginia further behind in ensuring children and their families have access to affordable and comprehensive health coverage.
Help more Virginia families learn about children’s health coverage options by spreading the word using DMAS Back to School resources.
