March 22, 2023
Will Virginia Maintain its Health Coverage Progress? To Be (Re)determined
Virginia’s choice in 2018 to expand Medicaid has served as a critical safety net for Virginians during the pandemic as shown by increased health coverage rates over the last few years. Since Virginia’s expansion of Medicaid was implemented in January 2019, the share of Virginians without health insurance has dropped two full percentage points to a historic low of 6.8%, down from 8.8.% in 2018 and 730,000 adults currently have health coverage thanks to expansion. And parents becoming aware of eligibility for themselves and their kids has led to the highest children’s coverage rates in Virginia ever. The benefits of Medicaid expansion go beyond health coverage rates as a recent study showed that enrolling in the expanded program positively impacted people’s financial security. But without adequate resources, planning, preparation, and targeted outreach, Virginia’s progress could be halted.
An estimated 172,000 people in Virginia are expected to lose coverage despite remaining eligible in the year following the end of the “continuous coverage” provision with children, Latino, and Black individuals being harmed the most. State policymakers can protect and build on Virginia’s progress by supporting Virginia Department of Medical Assistance Service (DMAS) and Department of Social Services (VDSS) planning efforts, making sure it has the resources to communicate with eligible and currently enrolled Virginia residents so they can stay connected to appropriate coverage, and promote accountability by maintaining publicly available disaggregated data.
Background of “Continuous Coverage Provision”
At the start of the COVID-19 pandemic, the federal government enacted several policies to protect and increase access to comprehensive health coverage. In particular, the 2020 Families First Coronavirus Response Act established a “continuous coverage provision,” which meant that anyone who was enrolled in health coverage through Medicaid would be able to keep it without needing to undergo annual redetermination of eligibility. This policy has benefited hundreds of thousands of Virginia families by offering ongoing health coverage for people who have been enrolled or newly enrolled in Medicaid coverage since March 2020.
But when the continuous coverage provision expires on April 1, 2023, Virginia, like all other states, will need to begin reviewing and redetermining eligibility for all people enrolled in Medicaid, also referred to as “unwinding.” The major risk is that people who remain eligible for Medicaid are at risk of losing coverage if they do not receive clear and concise communication about the redetermination process and the required documentation needed to complete it. Others may need assistance transitioning to comprehensive health coverage like those offered on the Affordable Care Act (ACA) marketplace to avoid becoming uninsured.
Disenrollment of People from Medicaid, Despite Being Eligible
According to estimates from DMAS, anywhere from 14% to 20% of people currently enrolled in Medicaid could lose coverage once redeterminations resume, which is comparable to national projections of 17.4%. Using the most recently available Medicaid enrollment data, roughly 304,500 to 435,000 people in Virginia would be disenrolled from Medicaid coverage in the 12-month period of Medicaid unwinding.
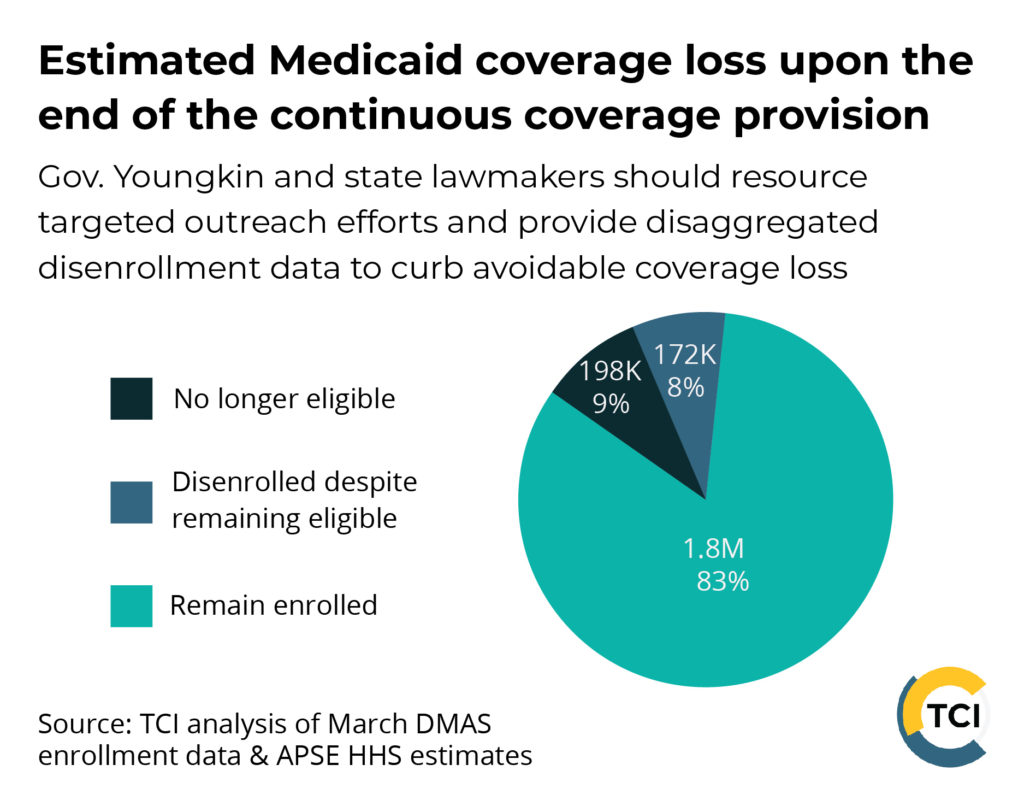
When considering a mid-range projection where 17% of Virginia’s total Medicaid enrollment — nearly 370,000 people — lose coverage, roughly 172,000 people would be disenrolled despite being eligible for coverage. In other words, an estimated 47% of people who lose coverage during unwinding will be disenrolled despite remaining eligible. Recent national analysis suggests children, Latino, and Black individuals are particularly vulnerable to being disenrolled while remaining eligible. In fact, 74% of children who lose coverage nationally are expected to be disenrolled despite remaining eligible. In addition, people who have moved, especially those who have faced several changes in mailing address due to housing instability exacerbated by the pandemic-fueled housing market, and people with limited English proficiency may be at greater risk of being kicked off of coverage.
Virginia lawmakers and the Youngkin administration can avoid the disenrollment of those who remain eligible by sufficiently funding and staffing targeted outreach and communications efforts. Local DSS offices that are responsible for implementing the eligibility reviews should be able to lean on state agencies and additional state funding to meet the caseload demands of the Medicaid unwinding process. The administration and state agencies should partner with trusted groups who have expertise working with communities expected to be most impacted. Clear and easy-to-read messages available in multiple languages currently instruct people enrolled in Medicaid to update their contact information in anticipation of the start of redeterminations in April and submit renewal paperwork to stay enrolled when the time comes to do so.
For targeted communications to immigrant populations, messaging should emphasize that Medicaid enrollment (except for the use of Medicaid to pay for long-term care in an institution like a nursing home) will not negatively impact people seeking a change in immigration status. Messages should also reassure people that their information will be kept private and be used only to redetermine their eligibility. VDSS and DMAS should also make sure that their staff meet client language needs and all federal requirements when handling calls and inquiries, sending notices, and meeting in person. Quality interpretation services should be available at any step of the redetermination process.
Virginia DMAS & VDSS have worked diligently to prepare for Medicaid unwinding but will need continued resources and dedicated staffing to effectively communicate, plan, and process redeterminations.
See DMAS Unwinding Toolkit for materials on how to spread the word.
Connecting Those No Longer Eligible to Coverage
For individuals who are no longer eligible for Medicaid, connecting them to other forms of comprehensive coverage such as through the Affordable Care Act (ACA) marketplace will be an important step in maintaining Virginia’s progress in connecting more people to health coverage. Thankfully, for people no longer eligible for Medicaid coverage, federal action will allow many to access ACA marketplace health coverage with low or no out-of-pocket premium costs.
As part of the American Rescue Plan of 2021, individuals purchasing health coverage through the ACA individual marketplace have received financial assistance through temporarily enhanced subsidies, which have lowered out-of-pocket premium costs for coverage. Nearly 308,000 Virginians signed up for marketplace coverage for 2022 — an increase of more than 17% over 2021 largely due to the subsidy expansion — according to the Kaiser Family Foundation. These subsidies were recently extended through 2025, expanding access to affordable coverage for the roughly 197,500 people who may be ineligible for Medicaid coverage in Virginia. People losing Medicaid coverage during the unwinding period will be allowed 60 days to enroll in ACA coverage thanks to a Special Enrollment Period in place through July 2024.
Conclusion
Adults and children across Virginia have benefited from continuous access to Medicaid coverage throughout the federal public health emergency. However, an estimated 172,000 people could lose health coverage despite remaining eligible for Medicaid and another 197,700 are at risk of not being connected to alternative coverage if Gov. Youngkin’s administration, state agencies, and lawmakers fail to plan and adequately resource outreach and communication efforts.
Children, Latino, and Black individuals are at higher risk of being disenrolled despite remaining eligible for coverage. Partnering with key and trusted organizations and messengers in impacted communities will be important to make sure people are made aware of and are able to complete the redetermination process in a timely manner. An unanticipated lapse in health coverage could cause serious health and financial harm on those affected.
Budget language from the 2022 legislative session directs the Secretary of Health and Human Resources to establish a “Task Force on Eligibility Redetermination,” which mandated a report to the governor and members of the legislative money committees by October 1, 2022, with regular updates until July 2023. The first report of this Task Force was published in November and subsequent briefings from the Secretary of HHR to lawmakers did not mention targeted outreach strategies to the most impacted communities.
Failure to detail and discuss obstacles to redetermining eligibility for parents of children enrolled in Medicaid and Latino, Black, and immigrant individuals indicates that the Youngkin administration and other key stakeholders involved in the task force have more work to do to avoid disproportionate coverage loss for these families. DMAS has proactively committed to publish public dashboards including data on disenrollments, successful renewals, and ongoing cases by race/ethnicity, coverage group, and gender. Continued access to these data will be key to monitoring unwinding in real-time.
These estimates are concerning but not an inevitability. The redetermination process will be a massive undertaking, but strong and vocal leadership and collaboration will help alleviate this burden on eligibility workers and help more Virginia families keep their health coverage.
If you or a loved one has health coverage through Medicaid, we encourage you to visit CoverVA.org or CubreVirginia.org (Spanish) to learn more about the return to normal enrollment and update your contact information to receive important updates and information.
Categories:
Budget & Revenue, Health Care
